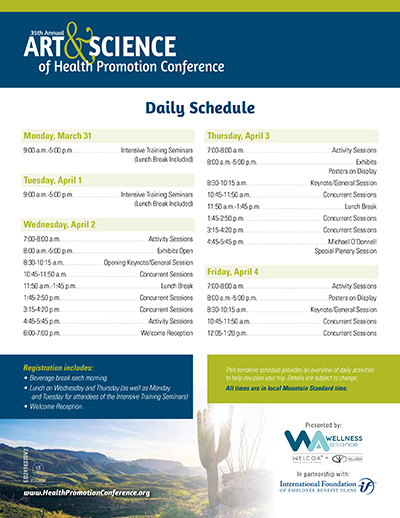
Conference Schedule
Why You Should Attend
- Join other health promotion and wellness professionals to learn, share and connect.
- Be inspired and equipped to bring new practices and approaches to your health promotion efforts.
- Find support in creating programs and resources that meet the needs of a diverse, multigenerational workforce.
- Learn strategies for raising awareness, building skills, and promoting policies and practices that foster population health and well-being, including more positive and supportive interactions.
Full Agenda
8:30 AM - 10:15 AM
Join Charles Vogl, adviser, speaker, and author of three books, as he delves into the essence of community and tackles the pressing issue of loneliness in the U.S. Through engaging discussions and practical insights from his books, Vogl will reveal the transformative power of the campfire experiences. Learn how to identify and create meaningful campfire experiences that foster deep, authentic connections among individuals, for in-person and virtual environments. This session is perfect for health promotion leaders, and anyone passionate about enhancing relationships and combating loneliness in their profession, organization, city or family.
10:45 AM - 11:50 AM
This interactive breakout session will guide participants through the crucial role of self-empathy as the foundation for empathy toward others, fostering clearer and more compassionate communication. Using the "Four Chairs" role-playing activity as well as feelings and needs cards, attendees will practice Nonviolent Communication (NVC) techniques, learning how understanding and caring for one's emotions and needs is vital for truly empathizing with others and communicating effectively. The session also introduces evidence-based self-care and resilience strategies through the Life Ideals model, which incorporates six core self-care practices: relaxation, thought restructuring/mental flexibility, social connection, sleep, physical activity, and nutrition. By prioritizing self-empathy and self-care, participants will discover how to improve both personal well-being and the quality of their communication in professional settings.
10:45 AM - 11:50 AM
In today's rapidly evolving work landscape, fostering a sense of belonging has never been more crucial. As remote and hybrid models become the norm, many employees grapple with feelings of isolation and disconnection. But what if there was a creative, fun way to transform your workplace into a thriving, connected community?
Join us for an innovative, experiential session that explores the synergistic power of mindfulness, music, and movement in creating a healthier, more supportive work environment. Led by an expert in health psychology and expressive therapies, this session will delve into research and practical strategies to combat loneliness, boost employee well-being, and increase creativity.
You'll discover:
- How to leverage mindfulness practices to foster presence and connection
- The surprising impact of music on social bonding and stress reduction
- Movement techniques that energize teams and promote cohesion
- Reduce anxiety and depression symptoms
- Enhance job satisfaction and engagement
- Improve cardiovascular health and pain management
- Decrease substance abuse rates
This is much more than PowerPoint-driven learning – Get ready to experience these practices firsthand! Through interactive exercises, you'll feel the immediate impact on your energy, health, and sense of connection. Learn how organizations are already implementing these strategies to:
Don't miss this opportunity to shape your workplace culture, improve health, and unlock the full potential of your team.
10:45 AM - 11:50 AM
Dr. Ron Goetzel will provide an update on the most recent workplace health and well-being research studies including those that address the controversy over whether these programs are effective across multiple outcome measures. He will also address the shift from a return-on-investment (ROI) rationale to one that emphasizes value-on-investment (VOI). The session will introduce the APIE model as a methodology to assess, plan, intervene, and evaluate the effectiveness of programs including business case development, program design, effective implementation, and rigorous evaluation. Controversial issues will be addressed, including why so many well-intentioned programs fail and what ethical standards need to be addressed in designing programs that satisfy the needs of employers and diverse employee populations.
10:45 AM - 11:50 AM
In this informative, thought provoking and engaging presentation, internationally recognized thought leader and keynote speaker Dr. Tyler Amell will explore the science of resilience and well-being as well as how these important considerations of workplace health impact rehabilitation, work disability, and overall employer health and well-being strategy.
Modern workplace well-being strategies are predicated on pillars such as mental, physical, social, and financial health approaches that combine to prevent injury and illness as well as promote and protect worker health from an integrated perspective. Workplaces are looking to better understand the health of their employees, particularly in relation to stress, anxiety, and depression, all critical aspects of mental health. These conditions become even more important when they intersect other pillars, such as physical, social, and financial health issues to create more complex, co-morbid, or poly-morbid conditions. These invariably complicate the work disability and rehabilitation process, resulting in costlier and longer duration impacts on workplace health and productivity. This session will cover the currently available applied scientific research evidence that builds upon our understanding of causation as well as intervention strategies that can help build healthier workplaces.
1:45 PM - 2:50 PM
Generational diversity is playing an increasingly larger role than at any other time in today’s workforce. Organizations and employers have a great opportunity to leverage the strengths of each generation across all ages to positively impact their workplace culture and bottom line, especially through inclusion with the aging worker. According to the CDC the number of people 65 years of age or older are not only working longer, they are also spending more time on the job than their peers did in previous years. Employees with higher workplace belonging show a marked increase in their willingness to recommend their company to others, receive greater increases in raises, and receive more promotions. Today’s older Americans tend to have higher education levels than older workers did in the past and are more likely to be employed than adults with less education. These older adults are healthier and less likely to have a disability than in the past decades making it possible to extend their working lives past what society had viewed as a traditional retirement age range.
This session will identify and analyze the dynamics that are experienced through stereotyping and discrimination, along with issues related to a lack of belonging by the aging workforce. Participants will identify a thorough understanding of the importance of creating a culture through belonging for not only healthy aging, but for building a sense of belonging in the workplace thereby creating healthier organizations through social cohesion of this population.
1:45 PM - 2:50 PM
Dr. Ron Goetzel will provide an update on the most recent workplace health and well-being research studies including those that address the controversy over whether these programs are effective across multiple outcome measures. He will also address the shift from a return-on-investment (ROI) rationale to one that emphasizes value-on-investment (VOI). The session will introduce the APIE model as a methodology to assess, plan, intervene, and evaluate the effectiveness of programs including business case development, program design, effective implementation, and rigorous evaluation. Controversial issues will be addressed, including why so many well-intentioned programs fail and what ethical standards need to be addressed in designing programs that satisfy the needs of employers and diverse employee populations.
1:45 PM - 2:50 PM
In this highly interactive breakout session, we will focus on four elements of effective teamwork: collaboration, communication, connection, and creativity. Through a dive into research as well as participation in experiential learning exercises that can “mitigate social stress and enhance interpersonal confidence,” we will practice these four elements in a low-stakes environment, so attendees leave with practical tools that are accessible, inexpensive, and require few materials (Seppänen and Toivanen, 2023). Attendees will be encouraged to let go of perfection and show up as their authentic selves. Attendees will be able to zoom out and see how the exercises and structure of this session fostered their own sense of connection and belonging within our group, as well as how they can bring these skills back to their role within their organization and their communities. This breakout session is not just for those in leadership positions. ALL employees can be leaders amongst their teams no matter what title they have, and ALL employees can use these skills to improve their interaction amongst their teams, which can improve engagement and productivity at work.
1:45 PM - 2:50 PM
Research has shown that zip code is a stronger predictor of health than genetic code, and local governments can significantly impact health. Through policies, budgeting, and programming, mayors and city councils can direct initiatives that ensure their residents have access to healthy food, safe physical activity, and mental health resources. Come learn about the Healthy Utah Community designation that provides an innovative way to help local government leaders understand the impact they have on health and engage them in health promotion. It disrupts the widespread belief among community leaders that health is solely a product of individual behavior as well as cultivates connection and collaboration across political denominations and sectors to achieve system-level change.
3:15 PM - 4:20 PM
There is a silence that persists and a stigma in our society surrounding grief. Grief is scary, it makes us sad, and it reminds us how little control we have. But all grief experiences deserve to be heard and honored. Grief matters and the voices of those grieving demand to be heard. The grief journey also offers a chance for connection and community building. Grievers often report feeling abandoned, isolated and misunderstood. Often, the communities most impacted by trauma and grief have been marginalized and (due to racism, poverty, and disinvestment) may lack grief support services. Community health workers (CHWs) are frontline public health workers who are trusted members of and/or have an unusually close understanding of the community served. This trusting relationship enables the workers to serve as liaisons between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery. As a CHW working in end-of-life care, the speaker will share why CHWs are uniquely positioned to begin important discussions of grief. A CHW's role as a cultural mediator and trusted messenger means that they walk with community members through loss and grief. This presentation seeks to share tools and skills needed to provide culturally affirming grief education and support. We all experience grief, but our experiences are unique and varied. Understanding the concepts of grief-informed care and collective community care can help us show love to those who are grieving and create shared spaces to honor grief.
3:15 PM - 4:20 PM
As health promotion professionals, one of our major responsibilities is to engage in ADVOCACY! Yet many of us are not quite sure what advocacy entails or where to begin. This session will cover all of the basics, including the difference between education, advocacy, and lobbying the three types of advocacy who can and cannot advocate and how to identify an emerging health issue that would benefit from a policy, systems, or environmental change (aka advocacy effort). Additionally, we will explore the importance of reviewing evidenced-based research and best practices to address the identified emerging health issue. We will discuss the importance of identifying partners and stakeholders that may support or oppose the advocacy effort along with how to identify resources and gaps in resources when planning advocacy efforts. Finally, participants in this engaging, hands-on session will walk away with a draft strategic plan to assist them in implementing an advocacy effort to address their identified emerging health issue.
3:15 PM - 4:20 PM
Join us for an engaging and insightful session, where we will redefine the landscape of team dynamics in healthcare. This session will start by defining psychological safety through a diversity lens, providing a comprehensive understanding of its crucial role in healthcare teams. We will delve into the intersection of intelligent failure and psychological safety, illustrating how embracing and learning from mistakes can foster a culture of growth and innovation. Discover proven strategies to build high-functioning healthcare teams grounded in psychological safety with a diversity lens. We will share practical tools and techniques to create an environment where all team members feel valued, heard, and empowered to contribute their best.
Sharing how to scale these concepts with the aid of content-expert practice facilitators, we will present an innovative pilot program, "Healthy Happy Teams," implemented across nine patient-centered medical homes in Rhode Island through the Care Transformation Collaborative (CTC-RI). Learn how stakeholders were engaged in the development and outcomes of this collaborative, which aimed to enhance high-performing healthcare teams through the principles of psychological safety within a diversity lens. Attendees will gain valuable insights, practical strategies, and real-world examples to apply in their own organizations, driving both individual and collective success.
3:15 PM - 4:20 PM
Companies and the vendors who serve them often struggle to quantify the value of seemingly abstract workforce attributes. Leaders want evidence that efforts to address such things as well-being, inclusion, engagement, connection, or belonging are worthwhile. Too frequently, decision-makers must rely on limited or piecemeal data showing a single, narrow outcome, such as satisfaction survey, turnover or injury. In this session, Dr. Lynch will demonstrate how a fully integrated data platform provides unique, comprehensive intelligence to decision-makers. Specifically, using a data platform covering multiple years and over 80,000 employees, she will highlight the ways team ratings of connection and belonging are linked to broad work outcomes including medical costs, absence, disability, workers compensation, performance, turnover and self-report measures. Additionally, the results will explore work, employee, team and environmental issues that are predictive of belonging and connection. Lastly, this session will describe the key elements that maximize the utility of a comprehensive business intelligence platform.
8:30 AM - 10:15 AM
In today’s rapidly evolving world, fostering hope, purpose, and belonging is essential for enhancing well-being in both community and workplace settings. This keynote examines these three fundamental drivers impacting individual and collective well-being, with a focus on actionable insights for health promotion professionals. Leveraging multi-generational data with a particular emphasis on GenZ we’ll explore how to cultivate these drivers and discuss science-backed strategies to address their unique needs. Attendees will gain a deeper understanding of the role that hope, purpose, and belonging play in promoting mental and physical health and leave equipped with practical tools to strengthen these pillars within diverse communities and workforces.
10:45 AM - 11:50 AM
Many employers make workforce mental health a priority, but focus solely on providing behavioral health benefits and tertiary-level interventions to treat mental health disorders and support people who are already struggling. Even when programs broaden to promote psychological well-being, this is often relegated to education and awareness, self-care tips, and encouraging workers to adopt better coping skills, so they can be more resilient in the face of challenges. While beneficial, these approaches alone do not address the systemic changes at the job, team, and organizational levels that are necessary for optimal results. Work-related stressors such as high job demands, low control, unclear performance expectations, and lack of social support are linked to negative outcomes for both workers’ mental health and organizational performance, including absenteeism, turnover, and employer reputation. Beyond simply reducing negative consequences, healthy work design has the potential to contribute positively to people’s overall well-being and drive organizational excellence. In this session, presenters will review common psychosocial hazards in the way work is designed and conducted, social and interpersonal aspects of work, and the work environment and outline methods you can use to assess and mitigate risks for your workforce. Participants will gain insights from best-practice case examples and discuss barriers, challenges, and practical solutions for creating a workforce mental health program that gets results.
10:45 AM - 11:50 AM
Join us for an inspiring session on the transformative potential of yoga and meditation with the Sadhguru Center for a Conscious Planet. Since 2021, our Long COVID Patient Wellness Program has provided free, evidence-based practices to address debilitating symptoms such as breathing difficulty, stress, and mood disturbances. This groundbreaking program integrates scientifically validated breathing techniques and guided meditation into a structured format, moving beyond traditional healthcare models that focus solely on pharmacological treatments. Long COVID affects approximately 10-30% of individuals who recover from acute COVID-19, leading to persistent symptoms that disrupt daily life and work across multiple sectors. In this session, we will illuminate how our program’s focus on fostering social connection and emotional support addresses these profound challenges, aligned with the conference theme of combating disconnection and enhancing well-being. You will delve into the program’s holistic components, including evidence-based wellness practices, and discover promising results from published research. We will also showcase our successful scaling of this model to support other patient communities, highlighting its remarkable adaptability and effectiveness. Additionally, we will explore the potential for applying these holistic practices beyond healthcare, such as in corporate wellness and educational settings. Discover how integrating yoga and meditation into diverse sectors can not only elevate overall well-being but also create meaningful connections, offering a sustainable and transformative approach to managing chronic conditions.
10:45 AM - 11:50 AM
Culture is a complex web of social influences on attitudes and behavior. Our health promotion goals for lasting change can best be achieved through a culture shift that establishes healthier attitudes and behaviors. We will examine social climate—a sense of community, a shared vision, and a positive outlook. These enabling factors generate the level of trust and openness that is needed to bring about complex cultural changes. We will then turn to the 15 cultural touchpoints that can strengthen new norms. These touchpoints include rewards, modeling, training, communication, traditions, relationship formation, and pushback. Working with social climate and touchpoints, we can go a long way towards creating the sustained healthy behavior changes that make health promotion programs thrive.
10:45 AM - 11:50 AM
In a world where mental health is paramount, Alexa’s session introduces AI as a transformative tool for workplace wellness. She begins with a visualization exercise, easing participants into embracing AI for efficiency and sustainability. Alexa addresses the pressing issue of burnout, offering strategies to alleviate stress and foster resilience. The session underscores the necessity of wellness initiatives, as employees increasingly prioritize their health. By implementing innovative wellness programs, organizations can enhance employee well-being, with data reflecting positive outcomes. The discussion highlights the rising demand for such programs and showcases successful examples of scaled wellness commitments. Alexa emphasizes the impact of workforce well-being on business sustainability, retention, and profitability. She explores AI’s role in managing staff wellness, leveraging data science to create evidence-based solutions and inform practices. AI’s analytical prowess is also harnessed to screen for mental health indicators, allowing for timely interventions. Ultimately, AI empowers organizations to tailor wellness strategies to their staff’s needs, fostering a healthier, more productive environment.
-
 Brett Powell, B.A., CWPC
Brett Powell, B.A., CWPC
1:45 PM - 2:50 PM
Belonging has been shown to be a critical driver of well-being, yet one in five employees report they don't feel like they belong when they are at work. Experiencing community and connection has a powerful effect on employee satisfaction, engagement and retention as well as individual health and wellness outcomes. In this session, we'll explore actionable steps organizations can take to foster a sense of belonging, supporting our human need to feel welcomed, valued, and respected.
Additionally, we'll examine a case study of an organization that embarked on a transformative journey to enhance its culture. The year-over-year results highlight the improvements achieved through intentional change, informed by data-driven strategies. We'll discuss the data collection process, the interventions implemented, and the outcomes achieved, as well as what went well, opportunities for improvement, and how leadership navigated challenging situations. This session will leave you energized and equipped with practical insights to enhance belonging within your organization.
1:45 PM - 2:50 PM
In the digital age, misinformation about health and wellness has become a significant challenge, impacting not only public health but also employee well-being. Studies show that misinformation can lead to poor health decisions, such as forgoing evidence-based treatments for unproven supplements or practices, which can have serious implications for employee health and productivity. This breakout session aims to equip attendees with the tools and knowledge to combat health misinformation within the workplace.
We will explore the psychological mechanisms behind susceptibility to health misinformation, including lack of awareness of being susceptible to poor health information, the influence of social media, and the role of cognitive biases. The session will also address specific examples relevant to corporate environments, such as the spread of false claims about diet, exercise, and mental health treatments. By leveraging scientific evidence and practical strategies, we will discuss how to identify and counteract misleading information, foster critical thinking, and promote a culture of informed decision-making.
Participants will leave with actionable insights and resources to develop educational initiatives, create supportive communication channels, and implement evidence-based wellness offerings to overcome health misinformation. These strategies will not only protect employees from the risks associated with misinformation but also enhance their overall well-being and engagement at work.
1:45 PM - 2:50 PM
Research indicates the severity of social disconnection and its impact on our well-being, but we lack a roadmap to help individuals, communities, and society at large create effective, sustainable change. In order to create a socially connected society, stakeholders from every sector and level of influence must recognize their role in this work and be equipped with evidence-based strategies. To empower these individuals to take action, the Foundation for Social Connection developed their SOCIAL Framework in collaboration with their multidisciplinary Scientific Leadership Council. Using this framework, they have published research reports exploring how to advance social connection across the lifespan in the health, education, work, built environment, and arts and culture sectors. In this topic presentation, attendees will explore evidence-based strategies that stakeholders of all backgrounds can employ to cultivate connection on the individual, organizational, community, and society level. Specifically, speakers will delve into findings from the work and built environment sector reports and allow the audience opportunities to share their experiences and thoughts on potential strategies to advance connection. Attendees will also emerge inspired by community examples of promising initiatives as well as knowledgeable of research and practice gaps requiring further exploration to improve our health and well-being.
1:45 PM - 2:50 PM
In this dynamic breakout session, participants will experience a rare blend of scientific insight, personal storytelling, and actionable strategies for living and working with purpose. Drawing from decades of research in behavioral science and his own journey into purpose-driven living, Dr. Strecher guides participants through a compelling exploration of how values, identity, and purpose can provide a new and powerful approach to workplace engagement and well-being.
3:15 PM - 4:20 PM
Integrate the concept of connection and community belonging as you engage more effectively in positive lifestyle improvement conversations with colleagues and the people you serve. This workshop will equip you with the methods and language for how to help people integrate connectedness into their action plans for lifestyle improvement and how to use the support of others to help them be accountable to themselves. By learning how to explore both the external and internal barriers to gathering support for lifestyle improvement we can help people learn how to ask for the help and support they need. We will explore the evidence for how a lack of community belonging for all age groups is associated with greater rates of heart disease, stroke, and many other physical ailments as well as its powerful impact on depression, anxiety, and suicide. Conversely, this session will reveal how a greater sense of community belonging can enhance both physical and mental well-being.
3:15 PM - 4:20 PM
In the post-pandemic era, creating a mentally healthy workplace is not just beneficial—It is essential. This session provides the insights and strategies needed to navigate this new terrain, paving the way for a workforce that thrives in the face of change. An analysis of the Household Pulse Survey data reveals compelling insights into how different work models affect anxiety, depression, and loneliness among employees. From fully in-person to hybrid and remote setups, each arrangement carries its own set of benefits and challenges. The research uncovers surprising trends in mental health issues across various demographic groups. It highlights the often-overlooked association between loneliness and broader mental health outcomes. This knowledge serves as a foundation for developing more effective workplace policies and interventions.
HR professionals, organizational leaders, and advocates for mentally healthy work environments will find this session indispensable. Attendees will gain a nuanced understanding of the complex interplay between work environment, social connection, and mental well-being. The session offers practical strategies for implementing hybrid work models and social connection initiatives, equipping participants with tools to foster a more resilient and connected workforce.
3:15 PM - 4:20 PM
Many organizations offer workforce wellness programs, benefits and resources that when utilized could theoretically help their employees make healthier decisions and contribute toward more positive emotions throughout the day. However, these assets have been largely individually focused. While admirable in its intent, this approach ignores the impact our co-workers, managers, and organization at large have on our ability to make healthy choices and keep a positive state of mind.
Companies and organizations need to move past the mentality of individual employee accountability for their health and well-being toward a partnership whereby the workplace and work system is supportive and conducive to making the healthiest choice the easiest choice, where our mental state is more easily able to flourish and less likely to be blemished by unfavorable events. This session will show how using an organizational assessment tool can provide the backbone of a strategic plan that helps shape an institution wide approach. While this session will highlight how the CDC Worksite Health ScoreCard was applied at Johns Hopkins Medicine for a decade, the participant can apply the lessons learned to their own institution and to use with other organizational assessment tools.
3:15 PM - 4:20 PM
We are bombarded with stories about war, famine, crime, climate disaster, social unrest, disease, lack of civility, and political divisiveness – delivered ad infinitum via Tik Tok, Instagram, X, Facebook, and other social media. It turns out that doom scrolling is not good for one’s mental health and well-being. Not only that, money, power, fame, stuff, and more stuff can’t buy happiness (beyond a minimum threshold, of course). Just look at Elon, Jeff, Mark, and Donald. So, what can make us happy? Friends, family, faith -- and wait for it -- work. Work can be a happy place when there is an intentional culture promoting mental health and well-being. What does it take? Psychosocially, instilling positive emotions, creating “flow,” highlighting organizational support, building bonding relationships, and communicating a sense of purpose. Add fun, and work becomes a fulfilling life experience, and of course, a way to pay bills.
The session will not just wax poetic. It will present findings from recent studies and literature reviews uncovering the sources and impacts of toxic work environments that cause distress and burnout. On the bright side, it will also offer solutions that extend beyond telling employees to “grin and bear it.” The session builds upon traditional psychosocial interventions aimed at enhancing resilience by introducing organizational and environmental stressors and solutions to improve the workplace. The session will recall a case study of protective factors shown to be effective in ameliorating stressors experienced by front-line hospital food service workers during the height of the COVID-19 pandemic. Finally, the session will conclude by answering the question, “what is Ron Goetzel thinking about and what are his solutions to the world’s problems?
4:45 PM - 5:45 PM
Community as Medicine is a joyful, high-vitality, heartfelt, intimate, playful, and dynamic exploration of physical, emotional, social, and spiritual well-being. Based on the work of Dr. Elizabeth Markle and Open Source Wellness, this experiential keynote aims to shift our approach from talking about health to experiencing wellbeing together in a way that rapidly generates a culture of authenticity, candor, and alignment. Prepare to move, laugh, connect, and reflect -— all while directly experiencing the model that's breaking down silos, achieving outstanding health outcomes, pioneering highly innovative partnerships, and scaling nationally via the YMCAs and related community-based organizations.
8:30 AM - 10:15 AM
Did you know that employees who have meaningful relationships at work are seven times more likely to be engaged in their jobs, take fewer sick days, collaborate more effectively, provide better customer service, and have higher loyalty to their companies? Belongingness is the number one factor for employee satisfaction, and creating a culture of belonging is an effective solution for decreasing turnover and increasing employee fulfillment.
In this dynamic and interactive program, social relationships expert and author of The Business of Friendship: Making the Most of Our Relationships Where We Spend Most of Our Time, Shasta Nelson provides a framework to evaluate belongingness within your teams and delivers practical tools to create and accelerate the high-trust and resilient relationships that boost employee productivity, retention, and profitability.
10:45 AM - 11:50 AM
Belonging is essential to individual well-being and organizational success, yet as a health promotion program or intervention, the skills, habits, and practices of belonging are often overlooked. To distill the actionable takeaways from this week’s conference, four featured experts will discuss how health promotion practitioners can bring belonging and connection to each individual and group they serve. This panel offers actionable strategies to create healthier, more inclusive environments. Attendees will be exposed to new ideas and innovative strategies, research-based insights, and a deeper understanding of the transformative power of belonging for individuals and in creating thriving, inclusive organizations.
10:45 AM - 11:50 AM
As a conference attendee, have you ever wondered if you are hearing anything truly groundbreaking? Persistent and pervasive challenges with physical, emotional, social, and financial well-being raise questions about the success of our efforts in health promotion in the past two decades. Despite concerted efforts of multidisciplinary scientists and practitioners, rates of obesity, anxiety, depression, burnout, loneliness, lack of social connection, financial distress, and disconnection from nature remain concerningly high.
This session will summarize the findings of a literature review that examines progress in health promotion literature from 2003 to 2023. A team led by three health promotion scholars is comparing the articles published in six top-tier health promotion journals (American Journal of Health Promotion, Health Education and Behavior, Health Psychology, Annals of Behavioral Medicine, American Journal of Preventive Medicine, and Health Promotion Practice) in 2003 to those published in 2023. Only articles relating to health behaviors or interventions will be included (i.e., no commentaries). The team will report on the evolution of the literature or lack thereof over the past two decades. The review considers theoretical and conceptual models, health behaviors, study design, methods, target populations, extent to which research addresses unmet social needs, single vs. multiple behavior change focus, study limitations, and proposed future research directions. Join us to reflect on insights about where we’ve been and where we are going as a field – as well as how we can accelerate our progress in the next five years.
10:45 AM - 11:50 AM
An increasing number of reports over the years illustrates the statistical and qualitative trends tracking the experiences of the U.S. workforce within organizational climates that either encourage or inhibit a healthy mental well-being. Psychological safety is an important topic to address because of its association with positive work environments and job satisfaction. Dr. Amy Edmondson defines psychological safety as a shared belief that a group is safe for interpersonal risk-taking. In addition to the definition, participants in this session will be introduced to the stages of psychological safety as an indicator for progression through multi-layered dynamic changes within a team’s journey.
Leadership has been found to have the most significant impact on staff’s perception of psychological safety. The exercises in this session will also guide participants on how to examine the impact of leadership on the culture, investigate the workforce’s perceptions of psychological safety, and utilize the tools to facilitate a culture of workforce well-being.
Strategic disruption is what happens at the intersection of status quo that upholds a system operating under toxic stress and the adoption of a new belief system that cultivates trust and an environment in which all members of the workforce can thrive. Understanding how psychological safety feels and looks will be part of the experiential learning exercises in this session. Participants will engage in practical application activities focused on securing psychological safety for themselves and facilitating it for others using boundary spanning leadership tools to create safety and foster trust.
12:05 PM - 1:20 PM
Connection is a powerful workplace attribute, but it can be difficult to explain or measure. Plus, leaders may not know how to create or change the level of connection on their teams. Fundamentally, connection is something we experience. In this session, Dr. Lynch will review the science of listening and how effective listening can increase performance, confidence, well-being and, yes, connection among teams. Content will explore the connection between listening and psychological safety.
Next, she will explain what it means to be an effective listener, how that is achieved, and how others respond to good listeners. Using information from Dr. Lynch's book, Get to What Matters, the session will also cover three specific skills and strategies that characterize effective listeners, empowering attendees to instantly encourage better connection.
12:05 PM - 1:20 PM
Many organizations offer workforce wellness programs, benefits and resources that when utilized could theoretically help their employees make healthier decisions and contribute toward more positive emotions throughout the day. However, these assets have been largely individually focused. While admirable in its intent, this approach ignores the impact our co-workers, managers, and organization at large have on our ability to make healthy choices and keep a positive state of mind.
Companies and organizations need to move past the mentality of individual employee accountability for their health and well-being toward a partnership whereby the workplace and work system is supportive and conducive to making the healthiest choice the easiest choice, where our mental state is more easily able to flourish and less likely to be blemished by unfavorable events. This session will show how using an organizational assessment tool can provide the backbone of a strategic plan that helps shape an institution wide approach. While this session will highlight how the CDC Worksite Health ScoreCard was applied at Johns Hopkins Medicine for a decade, the participant can apply the lessons learned to their own institution and to use with other organizational assessment tools.
12:05 PM - 1:20 PM
In this session, attendees will learn about older adults living with HIV or AIDS and issues associated with this unique population, especially for long-term HIV survivors. Physical and psychosocial burdens associated with HIV will be discussed, with emphasis on social isolation and loneliness, which is high among survivors. Presenters will describe the development of Experienced Escapades, a community-based program informed by Baumeister and Leary’s “need -to- belong” theory, to promote social connectedness within this group. Program impact on isolation, loneliness, and quality of life will be presented using evaluation data. Program sustainability, especially for non-profit entities, will also be discussed.
The content was great. I also enjoyed how friendly the other participants were and I was easily able to make friends with those I just met. Stephanie JonesAnders